French healthcare professionals are claiming that they are exhausted, particularly since the COVID19 episode. Patients are complaining that they are being treated like diseased organs rather than people during medical consultations that are becoming shorter and less frequent. And researchers are observing an increase in social and regional health inequalities. How can we move away from a vision in which health appears to be reduced to a hospital-centric system of diagnosis and treatment?
A health system suffering from a mono-curative, fragmented and short-term organisation
In the last century, the healthcare system was organised to meet the demand for hospital treatment for acute, accidental and unpredictable illnesses. This demand is being transformed with the rise of chronic diseases, the consequence of technological, epidemiological, demographic, economic, social and political changes.
Technological and epidemiological reasons
Early detection and advances in diagnostic techniques are increasing the number of people whose conditions do not require treatment as an absolute emergency. Such conditions are known generically as chronic diseases. Cancer, cardiovascular disease, diabetes, osteoarthritis, chronic obstructive pulmonary disease, as well as neurovegetative diseases, allergies, autoimmune diseases, depression, endometriosis, fibromyalgia and so many others: 10.7 million people are covered by the French Health Insurance system’s “Long-Term Condition” (ALD) mechanism. But in reality, more than 20 million people – or 35% of the population covered by the general health insurance scheme – require treatment for a chronic condition. And this figure is underestimated if we take into account people who do not go to the doctor and are unaware of their condition.
Demographic reasons
Chronic conditions affect one in two French people, with this figure rising to three in four in the over 65s. By 2040, the amount of people over 75 years of age in France will have increased by 15%, to 4.4 million. This population ageing will lead to a sharp increase in the number of people with chronic conditions, resulting in higher healthcare and hospitalisation costs. As people age, some may have to cope with several chronic conditions, such as kidney disease and depression.
Economic reasons
According to the French Department for research, studies, evaluation and statistics or DRESS (2022), France spent 12.3% of its GDP on healthcare in 2021. The country ranks second in the European Union behind Germany (12.8%), with the average being 10.5%. The French National Health Insurance system has estimated that healthcare spending linked to chronic conditions will amount to €104 billion in 2020, accounting for 62% of medical care expenditure. The costs of treatment and hospitalisation are rising. The costs of new targeted and personalised treatments are skyrocketing, while research is lagging behind in the search for mass-market – and therefore inexpensive – therapies.
Lifestyle-related social reasons
Our modern lifestyles, sedentary living, smoking, poor diet, over-use of alcohol or psychotropic substances, stress, over-exposure to the sun, etc., are the perfect recipe for the development of chronic diseases. In France, the costs of a sedentary lifestyle for the 20-70 years age bracket are estimated to be €1.8 billion a year, while the external costs (loss of production, cost of lives lost, loss of quality of life) are estimated to be €131.7 billion (Dervaux and Rochaix, 2022). The costs of care due to smoking-related illnesses are estimated to be €26 billion, with the external costs estimated to be four times higher (€105 billion). For alcohol, the figure is €8 billion, with external costs of €114 billion (Kopf, 2015).
Political reasons
In the last century, health policies focused on curing disease. The discovery of mass-produced medicines and medical devices played a major role in doubling global life expectancy over the course of the century, from 35 to 70 years. This improvement led people to believe that medicine would be all-powerful and capable of curing all illnesses. However, over the past 20 years, life expectancy has plateaued or even declined in some countries due to chronic diseases. Emergency treatment and curative measures alone are no longer enough to prevent problems.
Numerous reports, from the latest on the subject by France’s supreme audit institution, the Cour des Comptes, in 2021 to the first one produced by the WHO in 2006, call for a better balance between care and prevention. In France, the proportion of spending dedicated to prevention is estimated to be between 2 and 3%. Per capita, this expenditure represents less than €100 out of a total health expenditure of €4,500. It is mainly targeted at health promotion campaigns. While these do provide information, they do not bring about lasting changes in behaviour or lifestyles. Preventive initiatives in the workplace, in schools and targeting vulnerable, elderly or chronically ill people have been neglected. The gap has widened between professionals in the medical, social and educational fields, who pass the responsibility for preventive health back and forth between them, with no resources to back it up.
Rethinking health through multiple, coordinated, long-term solutions
Reconciling prevention and care, thinking globally
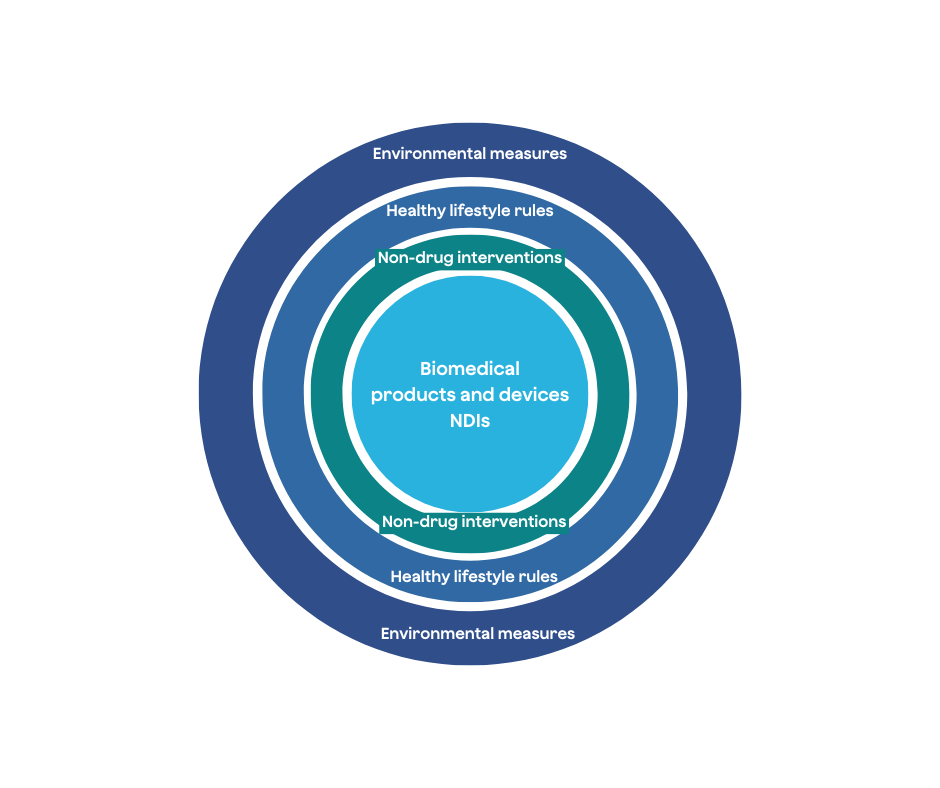
The old adage “prevention is better than cure” seems to have been forgotten by the biomedical industries encouraged by the transhumanists. Yet our century needs to invest in effective action at all levels: the environment, healthy lifestyle rules, non-drug interventions (NDIs) and medical products (Figure 1). Schools will play a key role in disseminating scientific knowledge of health-promoting actions. This knowledge will make it possible to combat all forms of obscurantism and misconceptions. The most widespread of these is the belief that an advertising message is enough to bring about a lasting change in the health behaviour of the entire population. NDIs, which are still little-known, will be one of the solutions for dealing with chronic conditions. An NDI is an “effective, personalised, non-invasive, referenced prevention or care protocol supervised by a qualified professional”. It corresponds to a predominantly psychosocial method (e.g. psychotherapy to combat sleep disorders or a programme to prevent injuries in high-risk working environments), a nutritional method (e.g. a diet to combat gastric disorders) or a physical method (e.g. a programme of adapted physical activity to combat lower back pain or a hydrotherapy treatment to combat osteoarthritis of the knee) implemented with all the ethical and relational expectations in a given health context by a professional (Ninot, 2019). The French Agency for Health Innovation is currently considering how to integrate these practices into its strategy.
Giving healthcare and prevention professionals the means to innovate
Professionals need to be given back the capacity to conduct research, practitioners the capacity to innovate, and patients the capacity to engage in an active and sustainable health approach. Restoring meaning and confidence in human beings who care for other human beings is going to be essential in this century. Without this, the door would be wide open to charlatans self-declared as the sole providers of benevolence and “care” via social networks.
By neglecting the reality of the systemic burden of chronic disease, health thinking has failed to consider prevention. Efforts must focus on extending healthy life expectancy for the population as a whole. This is all the more urgent given that the socio-economic impact of chronic conditions will have a delayed effect. Investment should be a public policy priority given that it is also an essential factor in economic growth. One of the major challenges of our century is to move beyond what made the last century such a success in the field of health: the curative approach. In the 21st century, we no longer have to deal only with hereditary and accidental diseases, but with complex, insidious diseases of behavioural and/or environmental origin. The prevailing techno-anxiety, social anxiety and eco-anxiety are only serving to further increase the number of people with chronic conditions. The solution will have to involve targeted, scientifically-based preventive health measures known as NDIs.
This article is extracted from one of the seven files of the Health Observatory PRO BTP; Our healthcare system. You will find other resources related to this study file here. PRO BTP has created the Health Observatory to support those who wish to take an active role in their well-being: understanding, preventing, and taking action on their health in everyday life. Chronicles, interviews, podcasts, videos... in partnership with a network of recognized experts and major national media, the observatory provides you with keys to understanding, practical advice, and concrete and innovative solutions, addressing a significant health topic each month. Selected for their importance to the French public, the topics are rigorously addressed by a scientific committee, recognized health experts and professionals, specialized journalists, to provide you with reliable and useful information in your daily life.
